
BENEFITS OF OUR AI
Direct impact on ROI, data health and NPS.
process claims
in minutes
instead of days
in minutes
instead of days
+ speed
handle growth
aND
peak volumes
aND
peak volumes
+ scalability
reduce overpayments
and
financial leakage
and
financial leakage
- fraud
avoid
human errors
in data entry
human errors
in data entry
- errors
ADAPTS TO YOUR BUSINESS
Built for control, not constraints
PRIVATE
In your own public cloud infrastructure or in M47’s but always ensuring maximum security, privacy, and regulatory compliance.
INTEGRATED
Fully integrates with your existing systems, including CRMs, ERPs, and other business platforms, ensuring seamless workflows and unified data management across all operations.
MONITORED
Continuously monitored in production to track performance, detect AI drift, identify errors, and ensure accuracy and reliability over time.
CUSTOMIZABLE
Tailored to fit your needs, because every company is unique. Underwriters, Assistance companies, TPA´s, MGA´s. Our AI adapts seamlessly to your processes.
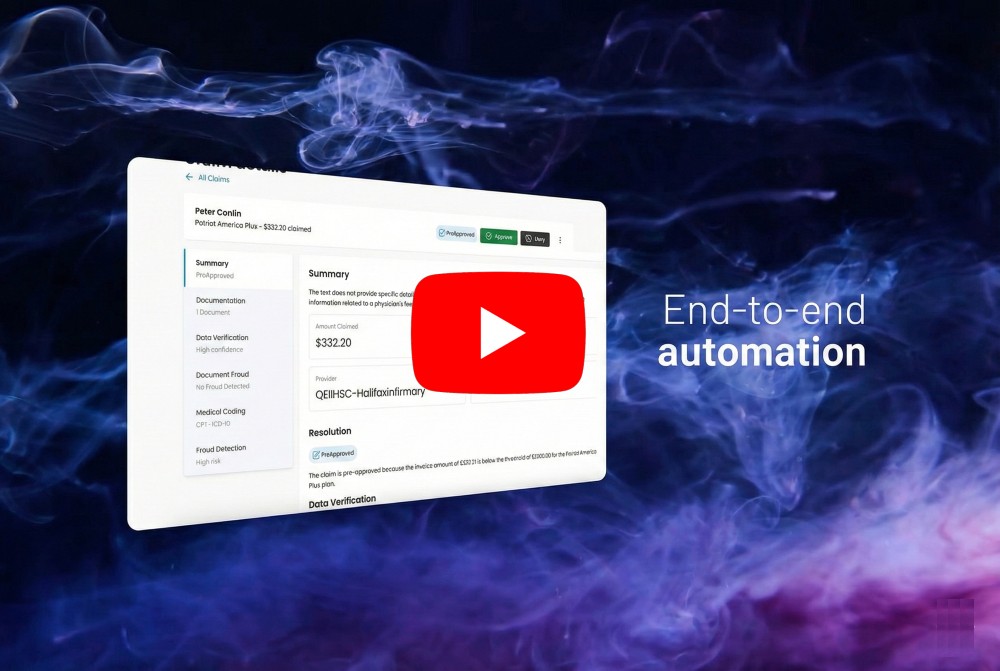
HOW IT WORKS
Less than 1 minute
Automating the claims journey from intake to resolution
Intake
Automates the capture, verification, and understanding of claim information from documents and unstructured data.
Validation
Normalizes, validates, and standardizes claim data by applying business rules, coding, and internal checks.
Fraud Detection
Identifies inconsistencies, document manipulation, and risk patterns across the claim lifecycle.
Resolution
Enables straight-through processing for standard claims and prepares resolution recommendations for human review.
Action
Executes post-resolution actions, including system synchronization, communications, and task guidance for agents.
Testimonials
What they say about us
"claims47 helped us transform a slow, manual process into something faster and more consistent. The AI system they helped us build assists our teams in reviewing medical forms, reducing human workload by up to 80%, while ensuring that final decisions remain in expert hands and fully comply with regulatory standards."
FEATURES
A bunch of AI capabilities that sits on top of your existing systems.
INTAKE
Smart Data Capture
Leverages advanced AI-powered OCR to extract key information from physical documents like PDFs and screenshots, accurately capturing complex layouts and tables.
Document Verification
Ensures that the right documents are uploaded for each claim. Using AI-powered analysis, it automatically classifies documents like invoices, medical reports, bank statements or national IDs, verifying that they match the required types for the claim.
Insightful Claim Summary
Uses AI to quickly and accurately summarize claims reports, extracting key details and providing concise overviews.
VALIDATION
Precision Data Matching
Ensures accuracy by validating extracted data against internal databases, such as matching provider names with hospitals.
Medical Coding
Automatically maps medical terms to standardized codes (e.g., ICD-10-CM, CPT), ensuring precise data representation with minimal manual intervention.
Data Structuration
Normalizes and structures unstructured information across documents, turning it into consistent, reliable data ready for validation, analysis, and integration with claims systems.
FRAUD
Document Fraud Detection
Leverages AI to identify fraudulent modifications in documents, such as altered invoice amounts or falsified details. AI-driven pixel-level analysis detects tampered areas in scanned documents, while autoencoder models flag anomalies by learning the typical structure of legitimate documents.
Fraud Detection
Leverages AI to analyze claim patterns and compare them against vast historical data to identify anomalies and inconsistencies.
RESOLUTION
Assisted Resolution
Applies coverage rules and verification logic to evaluate each claim, preparing clear, auditable resolution outcomes that support consistent and informed human review.
Straight-Through Processing
Automatically resolves standard, low-risk claims that meet predefined criteria, enabling straight-through processing for approved scenarios.
ACTION
Claims System Synchronization
Sends validated and structured data back to claims management systems such as Salesforce, ensuring systems remain up to date and aligned without manual re-entry.
Instant Communication
Automatically keeps claimants informed at every stage of the claims process through timely, personalized communications based on claim status and business rules.
Agent Communication and Task Guidance
Guides internal teams by surfacing required actions, next steps, and priorities, helping agents focus on exceptions and resolve claims more efficiently.
PLUS
Dashboard
Provides real-time visibility across the entire claims lifecycle through a web-based dashboard, enabling teams to monitor status, progress, and exceptions at a glance.
Machine Translation
Automatically converts key claim fields into the destination language set in the system. AI-powered language translation ensures accuracy, preserving critical medical, legal and technical terminology.
Currency Converter
Automatically converts invoice values into a predefined currency using real-time exchange rates. AI detects and normalizes currencies from symbols, abbreviations, and contextual clues, ensuring accurate conversions even in ambiguous cases.

Why us?
Over 20 years of experience in the insurance and tech world.We understand claims and AI, and we partner with major companies internationally to help their transformation journey.